Milk Allergy in Infants: Symptoms, Diagnosis, and Alternatives
A milk allergy in infants occurs when a baby’s immune system mistakenly identities proteins found in milk as harmful invaders. This triggers an allergic reaction, often involving the release of chemicals like histamine, which can cause a range of symptoms. The proteins responsible for the reaction are typically casein and whey proteins found in cow’s milk. Babies can also be allergic to milk proteins in breast milk if the mother consumes dairy products.
The immune response in milk allergy is an overreaction, and the symptoms can vary. It can range from mild symptoms like skin rashes to more severe symptoms, such as difficulty breathing or anaphylaxis.
Food allergies affecting your daily life?
Speak to a healthcare provider online about your allergy symptoms today.
Types of Milk Allergies in Infants
It’s important to differentiate a milk allergy from milk intolerance. While both conditions involve the digestive system’s response to milk, they are fundamentally different.
Milk allergy: This is an immune system response where the body treats milk proteins as harmful. Symptoms can affect the skin, digestive system, and even the respiratory system, making it a more complex and potentially dangerous condition.
Milk intolerance (lactose intolerance): This occurs when a baby’s digestive system cannot properly break down lactose, the sugar in milk, due to a deficiency in the enzyme lactase. The symptoms are primarily digestive, such as gas, bloating, and diarrhea, but do not involve the immune system. Lactose intolerance is generally less severe than a milk allergy.
Newborn milk allergy
Milk allergies in newborns occur when their immune systems react abnormally to proteins in milk, typically from cow’s milk or breast milk (if the mother consumes dairy). In newborns, the immune system is still maturing, which makes them more susceptible to developing allergies, especially to common allergens like milk proteins.
Newborns can develop milk allergies soon after birth. In some cases, this reaction happens when they are first introduced to formula, which often contains cow’s milk protein. Alternatively, if a breastfeeding mother consumes dairy, trace amounts of cow's milk proteins can pass through her milk to the baby, causing an allergic reaction in sensitive infants.
While the exact cause is not always clear, genetic predisposition plays a significant role. If a family has a history of allergies or conditions like asthma, eczema, or hay fever, a newborn may be at a higher risk of developing a milk allergy.
Milk protein allergy in infants
Milk protein allergy in infants primarily involves two proteins found in cow's milk: casein and whey. These proteins are large molecules that, when introduced to a sensitive infant’s immune system, can trigger an allergic reaction. The body mistakenly sees these proteins as harmful invaders, which results in the production of antibodies, such as IgE (Immunoglobulin E). These antibodies cause the immune system to release histamine and other chemicals, leading to symptoms like rashes, vomiting, diarrhea, or even more severe reactions like anaphylaxis.
Casein: This protein is slower to digest and can trigger more delayed allergic responses.
Whey: A quicker-digesting protein that tends to cause more immediate reactions.
The severity of these reactions can range from mild symptoms, such as skin rashes, to life-threatening issues like breathing difficulties.
Cow milk protein allergy in infants
Cow milk protein allergy in infants is one of the most common food allergies in early childhood. Cow’s milk contains both casein and whey, which are the primary allergens responsible for triggering immune reactions. When infants with a milk protein allergy consume milk (either through formula or breast milk with dairy proteins), their immune system reacts to these proteins as if they were harmful pathogens.
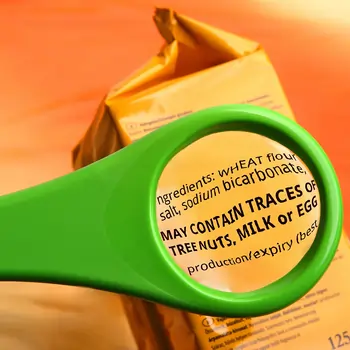
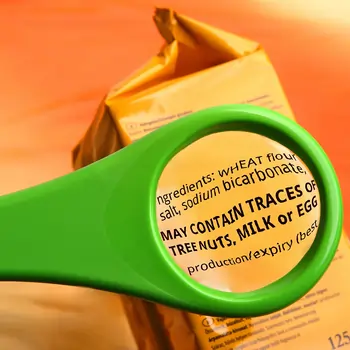
This allergy is most common in infants under 1 year old, as their immune systems are still developing. In many cases, babies may not tolerate even small traces of cow’s milk, which can be found in formulas, breast milk (if the mother eats dairy), or even processed foods that contain dairy ingredients.
Cow milk protein allergy may present as a variety of symptoms, such as gastrointestinal issues (vomiting, diarrhea, constipation), skin rashes, or respiratory symptoms. While some infants may outgrow their allergy by the age of three, others may continue to experience symptoms into childhood or even adulthood.
Managing a cow milk protein allergy in infants often involves eliminating dairy from both the infant’s and the breastfeeding mother’s diet, or switching to specialized hypoallergenic formulas. In more severe cases, avoiding all sources of milk protein becomes a lifelong necessity.
Milk Allergy in Babies: Causes and Risk Factors
Milk allergies in babies are often tied to a mix of genetic factors and environmental influences. If there’s a family history of allergies – whether it’s food allergies, asthma, or eczema – your baby might be at higher risk for developing a milk allergy too. Genetics play a big role in how your baby’s immune system responds to different proteins, including those found in milk.
Early exposure to cow’s milk or formula can also play a part. For babies who are introduced to cow’s milk-based formula too early or are exposed to milk proteins through breastfeeding (if the mom consumes dairy), their bodies may misidentify the milk proteins as harmful invaders, triggering an allergic reaction. So, it’s important to follow your pediatrician’s guidance on when and how to introduce milk products.
Recognizing the Signs and Symptoms of Milk Allergy in Infants
Milk allergy symptoms can vary widely depending on the severity of the allergy and the infant’s immune response. They may affect different systems in the body, including the gastrointestinal (GI), skin, and respiratory systems. It's essential for parents and caregivers to be aware of these potential symptoms to seek timely treatment.
Type of Symptom | Symptoms |
Gastrointestinal | Vomiting, diarrhea, constipation, abdominal pain, colic |
Skin | Eczema, hives, swelling |
Respiratory | Coughing, wheezing, difficulty breathing, sneezing |
Understanding rashes associated with milk allergies
Rashes are one of the most visible and common signs of a milk allergy in babies. These rashes can appear in different forms and may vary in severity, depending on the baby’s immune response.
Eczema: Often called atopic dermatitis, eczema is a skin condition that causes red, dry, inflamed patches of skin. Babies with milk allergies frequently develop eczema on their cheeks, arms, legs, or around the neck and chest. The rash is typically very itchy, and scratching can make the condition worse. Eczema may flare up shortly after exposure to milk protein, making it a strong indicator of a milk allergy.
Hives (urticaria): Hives are red, raised, and itchy welts that appear suddenly on the skin. These rashes typically develop within minutes to a couple of hours after milk consumption. They may be more noticeable around the face, mouth, or neck but can appear anywhere on the body. Hives can be a sign of a more immediate allergic response and may require quick intervention to prevent more serious symptoms.
Recognizing these symptoms early is essential for managing milk allergies in infants. If any of these rashes or other symptoms appear, it’s critical to consult with a pediatrician to confirm the diagnosis and begin a treatment plan. In cases of severe allergic reactions, such as swelling of the throat or trouble breathing, immediate medical attention is necessary.
Diagnosing Milk Allergy in Infants
When a milk allergy is suspected in an infant, pediatricians use several methods to make an accurate diagnosis. The process typically begins with a thorough medical history, including any family history of allergies, as well as a detailed account of the baby’s symptoms. If a milk allergy is suspected, pediatricians may use a combination of diagnostic tools, including skin tests, blood tests, and an elimination diet.
Skin tests
A common method for diagnosing milk allergies is the skin prick test. In this test, small amounts of cow’s milk protein are placed on the baby’s skin, usually on the forearm or back. The skin is then lightly pricked to allow the proteins to enter the skin’s surface.
If the baby is allergic to the protein, a raised bump (similar to a mosquito bite) will appear at the test site within 15-20 minutes. This test can help identify the specific proteins that are causing an allergic reaction, but it is not always suitable for newborns, so pediatricians may prefer other methods depending on the infant's age and health.
Blood tests
Blood tests can be used to measure the presence of specific antibodies, like IgE (Immunoglobulin E), which the immune system produces in response to allergens. If the baby’s blood tests show elevated levels of IgE in response to milk proteins, it may indicate a milk allergy. These tests are useful in identifying immediate-type allergic reactions, but they may not always be able to identify delayed reactions that can also occur in milk allergies.
Elimination diet
An elimination diet is a practical approach to diagnosing a milk allergy. If a milk allergy is suspected, pediatricians may recommend that the baby be temporarily removed from milk (either through formula changes or by eliminating dairy from the breastfeeding mother's diet).
After a few weeks, if symptoms improve, milk can be reintroduced under medical supervision to see if the symptoms reappear. This process helps confirm whether milk is the cause of the allergic reactions. For infants, this approach is usually combined with other tests to rule out other potential causes.
Dealing with Milk Allergy Rash Baby: What You Can Do
If your baby has a milk protein allergy, dealing with the rash can be tough, but there are things you can do to help. First, if your newborn has been diagnosed, it's essential to work closely with your pediatrician to figure out the best feeding plan. For breastfeeding moms, this may mean avoiding dairy in your own diet. If you’re using formula, your doctor might suggest a hypoallergenic one that’s easier on your baby’s system.
When it comes to soothing those rashes, it’s all about keeping their skin as comfortable as possible. Opt for gentle, fragrance-free creams or ointments to ease the itching and dryness, and be sure to moisturize regularly. Avoid anything that might irritate the skin further, like harsh soaps or tight clothing.
If the rash doesn’t seem to improve or gets worse, it’s a good idea to check in with your pediatrician. They’ll help you figure out if something else is going on or if a stronger treatment is needed.
When to Seek Medical Help
If your baby has a milk allergy, it’s important to know when to act fast. Severe reactions can happen quickly.
If your baby has trouble breathing, swelling around the lips, tongue, or throat, or seems faint or weak, it could be anaphylaxis. This is a medical emergency – get help immediately.
If your baby is having difficulty breathing or wheezing, it's crucial to seek emergency care right away.
For ongoing care, a pediatrician will be your best guide. They'll help manage your baby's diet, suggest safe feeding options, and track how the allergy might change over time. They’ll also know when to refer you to a pediatric allergist if needed.
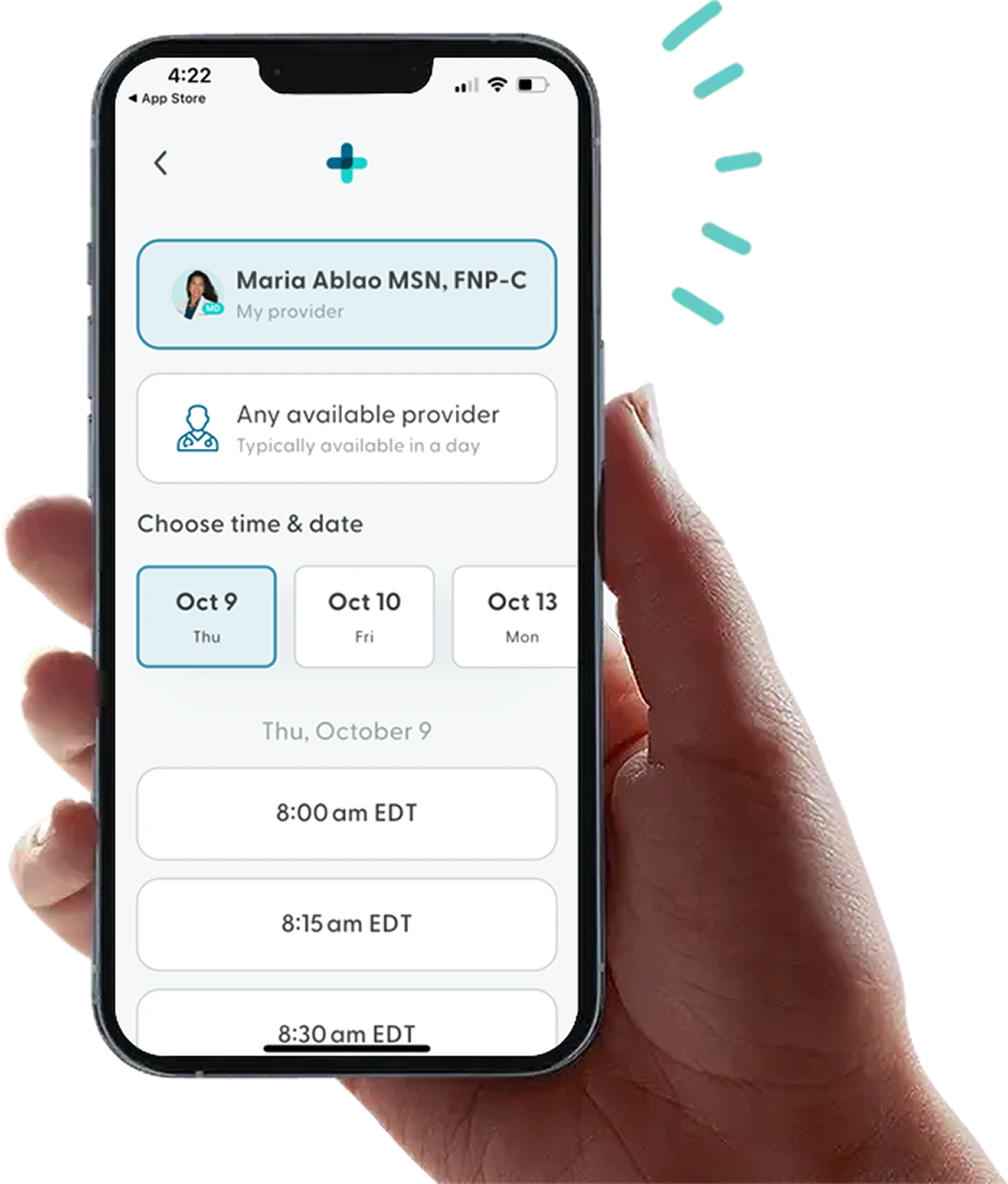
While LifeMD does not treat babies, we’re here for adults with allergies. A licensed healthcare provider can give you tips for keeping yourself safe during an allergic reaction and safe foods to add to your diet.
Make an appointment today to learn more about managing allergies.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD for seamless, personalized care — combining expert medical guidance, convenient prescriptions, and 24/7 virtual access to urgent and primary care.
 Medically reviewed and edited by
Medically reviewed and edited by 








