Shellfish Allergy 101: Shrimp, Lobster, and More
If you have a shellfish allergy, you’re not alone – it’s one of the most common food allergies, and reactions can range from mild discomfort to serious, life-threatening symptoms. Whether you’ve experienced a reaction before or just want to learn more, understanding what causes a shellfish allergy, how to recognize symptoms, and which foods or medications to avoid can help you stay safe.
There’s also a lot of confusion about whether people with a shellfish allergy need to avoid iodine or certain medical treatments, so we’ll clear up those misconceptions too. Here’s your guide to everything you need to know about shellfish allergies and how to manage them.
Food allergies affecting your daily life?
Speak to a healthcare provider online about your allergy symptoms today.
What is a Shellfish Allergy?
A shellfish allergy is an adverse immune response to proteins found in certain marine animals, primarily crustaceans (shrimp, crab, lobster) and mollusks (clams, oysters, scallops). When someone with this allergy consumes or, in some cases, comes into contact with shellfish, their immune system mistakenly identifies the proteins as harmful and releases histamines and other chemicals, leading to allergic symptoms.
Shellfish allergy is one of the most common food allergies in adults and can develop at any age, even in individuals who have previously eaten shellfish without issues. Unlike some childhood food allergies that are often outgrown, shellfish allergies tend to persist for life. Risk factors include:
Family history: Having relatives with food allergies increases the likelihood of developing a shellfish allergy.
Age: While it can develop at any age, it is more common in adults.
Previous reactions: A mild reaction in the past may indicate a higher risk for a severe reaction in the future.
Other allergies: People with a history of allergic conditions, such as asthma or other food allergies, may have a higher risk of developing a shellfish allergy.
Types of Shellfish Allergy
Shellfish allergies are generally divided into two categories based on the type of shellfish that triggers a reaction: crustacean allergies and mollusk allergies. While some people are allergic to both groups, others may only react to one.
Key Point: Crustacean vs. Mollusk Allergies
- Crustacean allergy: The most common and typically more severe type, with reactions often triggered by shrimp, crab, and lobster. Other allergenic crustaceans include crawfish and krill.
- Mollusk allergy: Less common and includes reactions to clams, mussels, oysters, and scallops. Other allergenic mollusks include squid (calamari), octopus, and snails (escargot). Some individuals allergic to crustaceans can tolerate mollusks, but cross-reactivity is possible.
Because crustaceans and mollusks belong to different biological groups, being allergic to one does not necessarily mean an allergy to the other. However, cross-contamination is common in food preparation, so those with a shellfish allergy are often advised to avoid both unless an allergist confirms otherwise.
Recognizing Shellfish Allergy Symptoms
Recognizing a shellfish allergy starts with understanding how the body reacts to exposure. Symptoms can range from mild to severe, appearing within minutes to a few hours after consumption.
Mild reactions may include itching, hives, nausea, or a stuffy nose, while more severe allergic responses can involve swelling of the face or throat, difficulty breathing, dizziness, or even anaphylaxis – a life-threatening reaction requiring immediate medical attention. The duration of symptoms varies; mild cases may resolve within a few hours, but more serious reactions can last longer and may require medical treatment to subside.
Medications to Avoid with Shellfish Allergy
People with a shellfish allergy typically do not need to avoid most medications, but certain substances have raised concerns due to potential cross-reactions. One commonly mentioned ingredient is chlorhexidine gluconate, an antiseptic used in medical settings and oral care products.
While not directly related to shellfish, some reports suggest possible hypersensitivity in individuals with food allergies. Additionally, iodine-based contrast dyes, once thought to be unsafe for those with shellfish allergies, have been debunked as a risk, as the allergy is linked to proteins in shellfish, not iodine. However, anyone with a severe allergy should inform their doctor before undergoing procedures involving contrast agents or antiseptics to ensure a safe treatment plan.
Shellfish Allergy Treatment and Management
Managing a shellfish allergy involves both emergency treatment and long-term strategies to prevent exposure. In the event of a reaction, epinephrine is the first-line treatment for severe symptoms like swelling, difficulty breathing, or anaphylaxis, while antihistamines may help with mild reactions such as itching or hives.
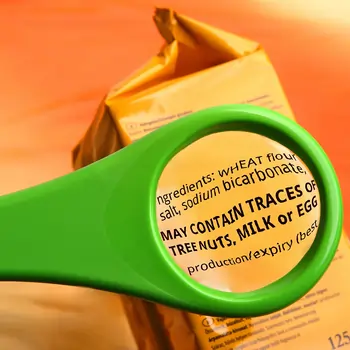
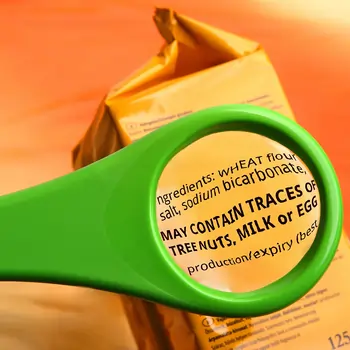
Long-term management includes strict avoidance of shellfish, careful label reading, and asking about ingredients when dining out. Those with a history of severe reactions should carry an epinephrine auto-injector at all times. It’s crucial to seek immediate medical help if symptoms escalate rapidly, especially if breathing difficulties, swelling of the throat, or dizziness occur, as these can indicate a life-threatening reaction.
Shellfish Allergy vs. Iodine Allergy
The belief that a shellfish allergy is linked to an iodine allergy is a common misconception. This idea stems from the fact that shellfish contain iodine, leading to concerns that people with a shellfish allergy may also react to iodine-based contrast dyes used in medical imaging. However, research has shown that shellfish allergies are caused by proteins (tropomyosin), not iodine, meaning there is no direct connection between the two.
People with a shellfish allergy do not have an inherently higher risk of reacting to iodine-based contrast agents. Similarly, chlorhexidine gluconate has been questioned for potential cross-reactions, but there is no established evidence linking it specifically to shellfish allergies. While any substance can trigger an allergic reaction in sensitive individuals, iodine itself is not an allergen, and people with shellfish allergies can typically tolerate iodine-containing products without issue.
Where Can You Learn More About Common Food Allergies?
At LifeMD, you can speak with a licensed healthcare provider about what to do if you suspect you’re allergic to shellfish. They can give you tips for keeping yourself safe during an allergic reaction and alternate food options to consider.
Make an appointment today to learn more about managing a shellfish allergy.












