Hormone Replacement Therapy (HRT): What are the Benefits and Risks?
Highlights
-
Hormone replacement therapy (HRT) is a treatment method that helps to relieve symptoms of menopause.
-
HRT works by restoring the body’s natural balance and replacing hormones that decline during menopause.
-
There are different types of HRT, including estrogen-only, progestin or combination therapy, and bioidentical hormones.
-
Each type of HRT has different benefits and risks, and your doctor will help you choose the most appropriate type for your situation.
Hormone replacement therapy (HRT) is a treatment option that is intended to help women manage uncomfortable symptoms associated with menopause.
It’s generally an effective way to significantly improve a woman’s quality of life during menopause.
However, because there has been confusing and often conflicting information about HRT over the past 20-25 years, it’s especially important to understand what the actual risks are based on current evidence.
Understanding Hormone Replacement Therapy
HRT is a treatment approach that involves supplementing or replacing hormones like estrogen, progesterone, and testosterone.
Menopausal hormone therapy (HRT) is used to ease common symptoms of menopause, such as hot flashes, mood changes, and vaginal dryness, by replacing some of the hormones that naturally decline during this time.
Beyond symptom relief, many people also use HRT to help protect their bones. Estrogen is essential for maintaining bone density, and when levels drop in menopause, the risk of osteoporosis and fractures increases. Restoring estrogen with HRT can help slow bone loss, support bone strength, reverse osteoporosis and reduce osteoporosis risk.
By smoothing out hormone fluctuations, HRT can also help stabilize mood and improve overall quality of life, helping individuals feel more like themselves again.
While HRT can be very helpful for managing menopause symptoms, some side effects can show up as your body adjusts to estrogen and progesterone. These may occur early on but often improve or resolve once your dose is fine-tuned and you reach your optimal regimen. These may include:
Acne
Bloating
Swollen and tender breasts
Headaches and migraines
Nausea
Vaginal bleeding
Mood changes
HRT side effects usually resolve on their own and will disappear after a few weeks. If any adverse reactions persist, speak to your doctor about adjusting your dosage.
Key Point: Who Should Avoid HRT?
HRT may not be a suitable solution for everyone. Women with a personal history of hormone sensitive cancers should speak to their healthcare provider about their potential risks.
Types of Hormones Used in HRT
There are several types of hormones used in HRT to address imbalances and symptoms associated with menopause.
Estrogen
Estrogen is the primary hormone used in HRT. It mimics the naturally occurring substance in your body.
This type of HRT – also known as estrogen therapy or estrogen replacement therapy – can be administered in various forms, including tablets, creams, patches, injections, gels, and vaginal rings.
It’s recommended to use a type of estrogen that can be applied directly to the skin because this method is associated with fewer side effects.
Topical estrogen – such as creams, gels, or patches – bypasses first-pass metabolism in the liver, which significantly reduces its impact on clotting factors and other liver-mediated pathways. As a result, transdermal estrogen is generally associated with a lower risk of blood clots and estrogen-triggered migraines compared with oral estrogen, while still providing effective symptom relief.
Progestin or combined hormone therapy
Progestin is a synthetic form of progesterone and can be prescribed with estrogen. This is why it’s also known as combination HRT.
Women who still have a womb should use estrogen alongside a progesterone or progestin to lower the risk of endometrial cancer.
This type of HRT can be taken orally, in a cream, or through an intrauterine device (IUD).
Research has shown that synthetic progestins (like those used in some older forms of hormone therapy and certain birth control formulations) are associated with a higher risk of breast cancer and blood clots compared with using estrogen alone or combining estrogen with bioidentical progesterone.
Progestins can more strongly stimulate breast tissue and can have less favorable effects on clotting factors and blood vessels, which is why combined estrogen-progestin therapy in large trials (like the original WHI) showed increased rates of breast cancer and venous thromboembolism. Because of this, many modern menopause protocols now favor bioidentical micronized progesterone over synthetic progestins when possible, to help lower these risks while still protecting the uterine lining.
Side effects of using progestin include:
Bloating
Headaches
Mood swings
Fatigue
Bioidentical hormones
Bioidentical hormones are derived from natural sources and mimic the chemical substances in your body. They are available in different forms, including creams, gels, patches, tablets, injection, and pellets.
These hormones are associated with a lower breast cancer risk and may be a safer option than synthetic alternatives. Bioidentical HRT also doesn’t affect blood clotting.
Benefits of Hormone Replacement Therapy
There are many benefits of using HRT, in addition to alleviating the symptoms of menopause and preserving bone health. These may include:
Improved cognitive functioning: Hormonal changes during menopause can affect cognitive abilities like memory and concentration. HRT has shown potential in improving these functions and reducing the risk of cognitive decline. This may also lower the chances of developing degenerative diseases such as dementia.
Enhanced mood and well-being: Hormonal fluctuations during menopause often lead to mood swings, irritability, and anxiety. HRT can help stabilize hormone levels, which may lead to an improved mood and an increase in overall well-being.
Prevention of certain health conditions: HRT has been associated with a reduced risk of developing certain conditions, including colon cancer, heart disease, and diabetes. This is especially true for individuals who start HRT close to the onset of menopause.
Cardiovascular Health. When started within about 10 years of the last menstrual period (LMP) or before age 60, menopausal hormone therapy appears to have neutral to beneficial effects on the cardiovascular system for many women. This is often called the “timing hypothesis” or “window of opportunity.” In this earlier window, estrogen can help improve lipid profiles, support endothelial (blood vessel) function, reduce central fat gain, and lower insulin resistance, which together may reduce the risk of coronary heart disease and overall mortality compared with women who never use HRT or start much later in life. In contrast, starting HRT more than 10 years after menopause or after significant atherosclerosis is already established may not provide the same cardiovascular benefit and can even increase risk in some women when over 20+ from menopause, which is why modern guidelines emphasize starting HRT – when appropriate – closer to the menopausal transition and with careful, individualized risk assessment.
While there are many benefits of HRT, the decision to start treatment should be made with your doctor.
Risks and Considerations of Hormone Replacement Therapy
Before starting HRT, it’s essential to be aware of the risks associated with this type of treatment.
For many women, the benefits tend to outweigh the risks.
Cardiovascular health
The relationship between certain types of hormone therapy and cardiovascular health isn’t fully understood yet.
Clinically, all evidence is typically distilled into a simple timing framework:
0-10 years from menopause: The “window of opportunity”: lower cardiovascular risk and possible benefit when using appropriately selected hormone therapy, especially as supported by trials likeELITE and early-initiation data from DOPS, as well as meta-analyses summarized by Hodis & colleagues. PubMed+2BMJ+2
10-20 years from menopause: A more neutral or uncertain zone, where the cardiovascular effects appear less clearly beneficial and depend heavily on individual risk factors and baseline vascular health, as reflected in WHI re-analyses and contemporary reviews.
>20 years from menopause: Generally considered a higher-risk period to initiate systemic HRT, with guidelines like the 2022 NAMS Position Statement noting a less favorable benefit-risk ratio and higher absolute risks of CHD, stroke, and VTE when started this late.
Endometrial cancer risk
Endometrial cancer develops in the lining of the uterus and typically occurs when a person is exposed to estrogen without the balancing effect of progesterone for a prolonged period.
It’s common practice to not recommend treating with estrogen only therapy if you still have a uterus.
Other considerations
There are a few other factors to consider before starting HRT. These include:
Increased risk of developing gallbladder disease: Estrogen used in HRT can increase a person’s risk of developing gallbladder issues. It’s recommended to report any symptoms of conditions like gallstones to your healthcare provider as soon as possible.
Impact on breast density: HRT has been associated with increased breast density, which can make mammogram screenings more challenging and impact its ability to detect cancer. To avoid this, your doctor may recommend regular breast examinations to help them monitor any changes or abnormalities.
Ongoing monitoring of these HRT risks is important for addressing any health concerns early on.
Key Point: Will HRT Make You Gain Weight?
Many individuals might be concerned that HRT will lead to uncontrollable weight gain. However, there is currently no evidence to support this.
Hormone replacement therapy (HRT) can sometimes cause a small amount of weight gain in the short term, but this is usually due to fluid retention rather than true fat gain. As your body adjusts to estrogen (and sometimes progesterone), you may notice temporary bloating, puffiness, or a tighter waistband – especially around the belly, hips, or breasts. For most people, this settles down over a few weeks to months once hormone levels stabilize and the dose is dialed in, and it doesn’t translate into ongoing, progressive weight gain.
Weight gain in midlife is common among men and women, regardless of any medical treatment they are receiving.
Eating a healthy diet and maintaining a good exercise regime can help manage excess weight.
You can also contact the qualified doctors at LifeMD to help you create a personalized weight management program.
When Should You Stop Taking HRT?
There is no limit to how long you can take HRT, so it’s recommended that you speak to a doctor to determine what would be appropriate for your circumstances.
The benefits you gain from HRT – such as symptom relief, better sleep and mood, and protection of bone density – are not permanent if therapy is stopped. Once HRT is discontinued, hot flashes and other symptoms can return, and bone loss typically resumes at a postmenopausal rate, which may gradually erode the gains you’ve made.
For this reason, HRT is usually thought of as a long-term strategy, not a quick fix. Maintaining a stable, well-monitored HRT plan and an ongoing relationship with your provider is the best way to preserve those benefits and adjust your dose safely over time as your needs change.
Key Point: Is HRT Safe?
Many medical professionals agree that HRT is generally a safe treatment option for most people.
However, HRT should only be used to treat specific conditions and can’t be used as a general medication.
This mainly includes experiencing menopausal symptoms or being at risk for developing osteoporosis.
Personalizing HRT and Seeking Medical Advice
When you’re deciding whether to start HRT or try an alternative, always consider what’s best for your needs.
It can be a difficult choice, which is why it’s always recommended to seek guidance from your healthcare provider.
They can help you determine the most appropriate HRT treatment regime based on your needs, medical history, and risk profile.
Your doctor can also monitor your symptoms and help detect any changes in your body that may be signs of underlying conditions.
Continuous monitoring is essential for preventing more severe diseases from developing or getting treated for them as soon as possible.
It’s also important to consistently evaluate the effectiveness of your HRT treatment with your doctor.
Where Can I Learn More About HRT for Menopause?
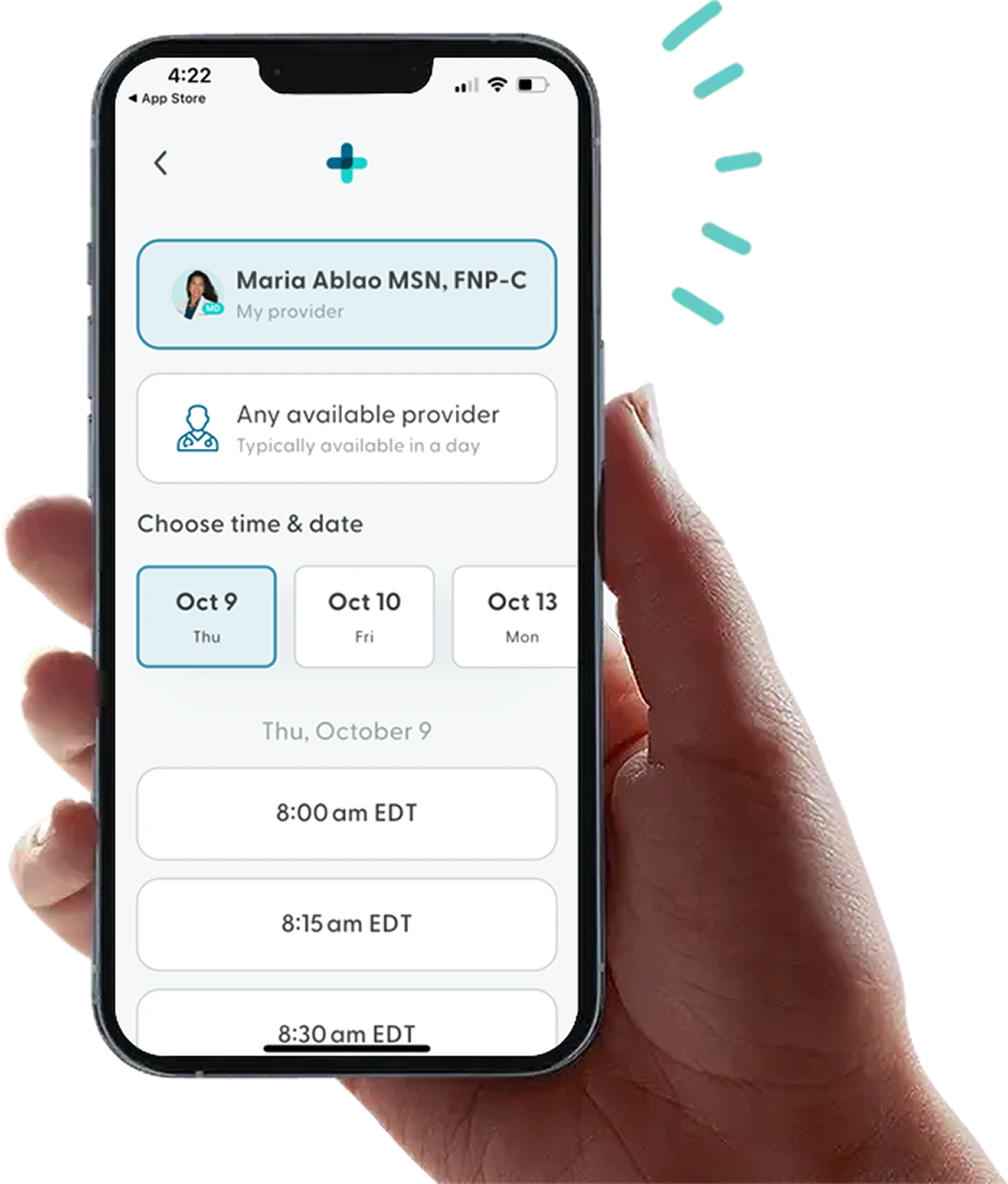
If you’re interested in learning more about HRT treatment, LifeMD can help.
The LifeMD Women’s Health Program is here to support you. Qualifying patients receive personalized guidance tailored to their experience, whether they’re navigating menopause or beginning to notice perimenopausal changes.
Schedule an appointment with LifeMD and get expert support for every stage of menopause – all from the privacy and comfort of your home.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD for seamless, personalized care — combining expert medical guidance, convenient prescriptions, and 24/7 virtual access to urgent and primary care.
 Medically reviewed and edited by
Medically reviewed and edited by 









