Milk Allergy vs. Lactose Intolerance: Understanding the Difference
When it comes to dairy, many people often mix up milk allergies and lactose intolerance, thinking they’re the same thing. But they’re actually quite different. Understanding the distinction is really important because the causes, symptoms, and treatments vary quite a bit.
Knowing the difference can help you figure out what’s going on and how best to manage it – whether it’s avoiding certain foods or finding the right treatments.
Food allergies affecting your daily life?
Speak to a healthcare provider online about your allergy symptoms today.
What is a Milk Allergy?
A milk allergy is when your immune system overreacts to proteins found in milk, like casein and whey. Instead of simply digesting the milk, your body treats these proteins as a harmful invader, triggering an allergic response. This can cause a range of symptoms, from mild skin reactions like hives or swelling, to more serious issues like trouble breathing or even anaphylaxis, which is a life-threatening reaction.
Milk allergy is most common in infants and young children, but some people might carry it into adulthood, although it’s less likely. For most children, though, a milk allergy tends to lessen with age. Still, if it does stick around, managing it is crucial to avoid severe reactions and keep your immune system in check.
What is Lactose Intolerance?
Lactose intolerance happens when your body has trouble digesting lactose, the sugar found in milk and dairy products. This is because your body doesn't produce enough of an enzyme called lactase, which is responsible for breaking down lactose in the digestive system. Without enough lactase, the lactose stays undigested and can cause a range of uncomfortable symptoms like bloating, diarrhea, gas, and stomach cramps.
Lactose intolerance is more common in adults, particularly in certain ethnic groups such as East Asian, African, and Native American populations. It can develop at any age, but it’s often seen in adulthood as the body’s production of lactase naturally decreases over time. While it's not life-threatening like a milk allergy, the symptoms can still be pretty unpleasant, making it important to manage your dairy intake or use lactase supplements to ease the discomfort.
Milk Allergy vs. Lactose Intolerance
The cause of a milk allergy lies in the immune system, where the body reacts to milk proteins like casein and whey as harmful invaders. This leads to an allergic response, which can cause a range of symptoms, from skin reactions to severe issues like anaphylaxis. In contrast, lactose intolerance is caused by a deficiency in the enzyme lactase, which is necessary to break down lactose, the sugar in milk. Without enough lactase, lactose remains undigested, causing digestive discomfort like bloating and diarrhea.
Symptoms comparison
When it comes to symptoms, milk allergy often triggers immediate reactions, sometimes within minutes of consuming milk. These reactions can be severe, including difficulty breathing or anaphylaxis, making it a potentially life-threatening condition. On the other hand, lactose intolerance tends to have a delayed onset, with symptoms appearing gradually, typically hours after consumption, and while uncomfortable, they are rarely severe.
Symptom | Milk Allergy | Lactose Intolerance |
1) Digestive discomfort | Rare | Common (bloating, diarrhea, cramps) |
2) Skin reactions | Hives, swelling, rash | Rare |
3) Respiratory issues | Wheezing, difficulty breathing | Rare |
4) Severe reactions | Anaphylaxis (life-threatening and immediate emergency care is necessary) | Not life-threatening |
Diagnosing Milk Allergy and Lactose Intolerance
Diagnosing a milk allergy typically involves either a skin prick test or a blood test. In a skin prick test, small amounts of milk proteins are applied to the skin, and the skin is then pricked to see if a reaction occurs. If the skin shows signs of an allergic reaction, such as swelling or redness, it suggests a milk allergy. A blood test can also measure the level of specific antibodies (IgE) in the blood that are produced when the immune system reacts to allergens like milk proteins.
For lactose intolerance, the diagnosis often includes the lactose tolerance test or the hydrogen breath test. In the lactose tolerance test, the patient drinks a liquid containing lactose, and blood sugar levels are measured over time. If the levels don’t rise as expected, it indicates that the body is not digesting lactose properly. The hydrogen breath test measures the amount of hydrogen in the breath after consuming a lactose-containing drink. Increased hydrogen levels suggest that lactose is not being digested and is instead fermented by bacteria in the colon, which leads to the symptoms of lactose intolerance.
Key Point: How DNA Tests Determine Lactose Tolerance
Believe it or not, your DNA can actually tell you whether you’re genetically predisposed to lactose intolerance. It all comes down to the LCT gene, which provides instructions for making lactase – the enzyme that helps break down lactose. Some people have variations in a nearby gene called MCM6 that control whether the LCT gene stays active into adulthood.
If you have the version that keeps lactase production going, you can likely enjoy dairy without issues. But if you have the variant that slows or shuts down lactase production your body struggles to digest lactose. DNA tests look for these genetic markers to help determine if your lactose intolerance is rooted in your genes.
Keep in mind that some people develop an intolerance towards lactose for other reasons too.
It’s important to consult a healthcare provider for an accurate diagnosis, as the symptoms of milk allergy and lactose intolerance can overlap. A proper diagnosis will guide treatment and help manage the condition effectively, whether it’s through dietary changes or medications.
Can You Have Both?
Yes, it’s possible to have both a milk allergy and lactose intolerance, though it’s relatively rare. When someone has both, it can complicate the diagnosis and treatment because the symptoms can overlap, especially when it comes to digestive distress after consuming dairy.
For instance, someone with a milk allergy might experience skin reactions, hives, or trouble breathing, while someone with lactose intolerance might only experience bloating, gas, or diarrhea. However, both can occur simultaneously, making it harder to pinpoint which condition is causing which symptoms.
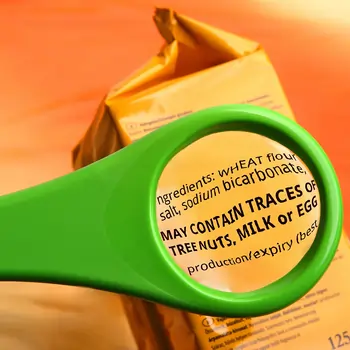
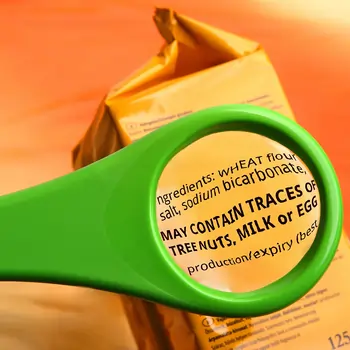
Managing both conditions can also be tricky. If someone is allergic to milk proteins but is also lactose intolerant, they’ll need to avoid all dairy products – since even lactose-free milk contains proteins that could trigger an allergic reaction. This means carefully reading labels and potentially working with a healthcare provider to find safe alternatives that avoid both the allergens and the lactose.
Treatment and Management
For those with a milk allergy, the primary treatment is strict avoidance of milk and milk products. This is crucial to prevent allergic reactions, which can range from mild to life-threatening. In cases of severe reactions – such as anaphylaxis – emergency treatment with epinephrine (often in the form of an EpiPen) is necessary to reverse the symptoms quickly. It's also important to work with a healthcare provider to develop a plan for managing potential allergic reactions, especially in situations where accidental exposure to milk might occur.
On the other hand, the treatment for lactose intolerance focuses on managing symptoms rather than eliminating the condition. Lactase supplements can be taken before consuming dairy to help break down lactose, making it easier to digest. Many people with lactose intolerance also find relief by switching to lactose-free dairy products or adjusting their diet to reduce lactose intake.
Tips for people with milk allergies
Choose substitutes like almond, soy, or oat milk, and be mindful of dairy-free alternatives.
Always read labels carefully, as milk can be present in unexpected products such as baked goods, processed foods, and even some medications.
Tips for people with lactose intolerance:
Opt for lactose-free dairy products, or try plant-based alternatives like almond or coconut milk.
If you can’t avoid lactose entirely, managing portion sizes and using lactase supplements can help alleviate symptoms and make dairy consumption more comfortable.
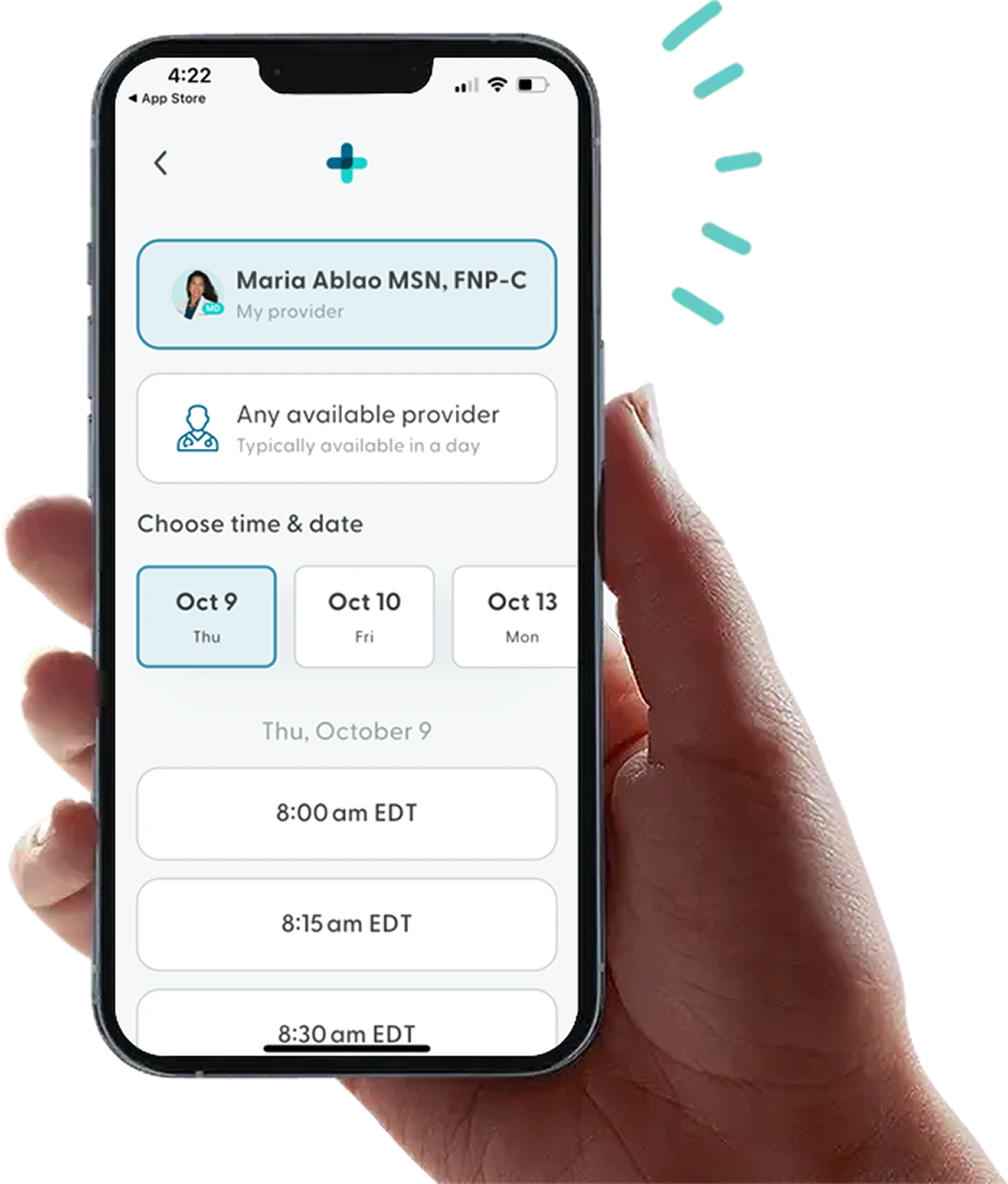
How LifeMD Can Help
At LifeMD, you can speak with a licensed healthcare provider about what to do if you suspect you’re allergic to milk. They can give you tips for keeping yourself safe during an allergic reaction and safe foods to add to your diet.
Make an appointment today to learn more about managing a milk allergy or lactose intolerance.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD for seamless, personalized care — combining expert medical guidance, convenient prescriptions, and 24/7 virtual access to urgent and primary care.
 Medically reviewed and edited by
Medically reviewed and edited by 








