Stages of Osteoarthritis of the Hip

Summary
- Osteoarthritis mainly affects older people, but it is possible for those in their 20s and 30s to develop the condition.
- There are four stages of osteoarthritis of the hip; treatment methods for the condition depend on which stage the person is in.
- It is easier to treat osteoarthritis in its earlier stages — but surgical interventions, such as hip resurfacing and total hip replacement, are required in severe cases.
- While there is no cure for osteoarthritis, it can be managed with exercise, proper diet, walking aids, and surgical treatments.
According to the Centers for Disease Control and Prevention (CDC), around 23.5% of U.S. adults have been diagnosed with arthritis. By 2040, it is estimated that 25.9% of Americans will have the disease.
Osteoarthritis (OA) is the most common type of arthritis in the U.S., and 32.5 million adults have the condition.
Other chronic conditions — or comorbidities — frequently accompany arthritis. These include obesity, diabetes, and heart disease.
It is estimated that the economic burden of osteoarthritis in the U.S. is $136.8 billion each year.
In this article, we’ll discuss the signs, symptoms, stages, and treatment options for osteoarthritis of the hip.
What is Osteoarthritis?
Sometimes referred to as a wear and tear condition or hip arthritis, osteoarthritis is a degenerative joint disease that mainly affects weight-bearing joints.
Osteoarthritis typically affects older people, and it’s one of the most common causes of disability among seniors. The condition is more prevalent in males younger than 45, but more common in women over 45.
The hands, neck, lower back, knees, hips, and feet are commonly affected by osteoarthritis.
Key Point: Can Osteoarthritis Affect Young People?
Although osteoarthritis is more common among older people, it is possible for those in their 20s and 30s to develop the condition.
However, if a younger person has osteoarthritis, there’s likely an underlying cause.
Some factors that can cause osteoarthritis in young people include:
- Joint injuries
- Repetitive stress or overuse of joints
- Being overweight
- A family history of the disease
- Poor posture
- Sitting for long periods
- A very athletic lifestyle or participation in high-impact sports
How Does Osteoarthritis Affect the Hip?
Osteoarthritis of the hip is characterized by the gradual breakdown of bone, cartilage, and hip tissue.
As one of the largest and strongest joints in the body, the hip is incredibly important for movements like walking, running, and jumping. In addition, the hips also stabilize our bodies, allowing us a greater range of motion.
The hip comprises a ball-and-socket joint. The rounded part of the hip joint is called the femoral head, and it fits into the hip socket, which is known as the acetabulum. Both the femoral head and acetabulum are covered in a slippery, flexible surface called articular cartilage.
In people with hip osteoarthritis, the articular cartilage that covers the ball-and-socket joint has worn down, subjecting the bones to increased stress. This can lead to the formation of bone spurs.
If someone has osteoarthritis they may experience pain or stiffness in the hip joint itself, or related areas, such as the thighs, buttocks, and groin.
Osteoarthritis may take years to develop. Over time, the condition causes increased pain and inflammation, as well as decreased hip mobility.
Key Point: What Are Bone Spurs, and How Are They Linked to Hip Pain?
Also known as osteophytes, bone spurs commonly occur due to hip osteoarthritis. They are hard bumps of extra bone that grow on the edges of the femoral head and acetabulum that form the ball-and-socket joint of the hip.
While bone spurs themselves aren’t painful, they can:
- Cause friction that leads to inflammation.
- Prevent the leg from rotating properly in its socket, thereby limiting the range of motion.
What Are the Symptoms of Hip Arthritis?
Because arthritis is a progressive disorder, it begins gradually and worsens over time. It’s also important to note that you may have mild osteoarthritis and not show any symptoms.
Early symptoms of hip osteoarthritis may include:
- Stiff hips
- Limited range of motion
- A clicking sound inside the hip
- Pain when the hip joint is strained; for example, when standing for a long period of time
Those with advanced or severe hip arthritis may experience the following symptoms:
- Pain whenever the hip joint is involved in movement
- Severe stiffness in the hip joint when waking up or moving around after a period of inactivity
- Loss of flexibility
- A grating or popping sound each time the hip joint moves
- Bone spurs (hard growths) that form around the hip joint
- Hip joints that are tender and swollen

What Are the Risk Factors Associated with Hip Osteoarthritis?
There are certain risk factors that leave people more prone to osteoarthritis. Some of these conditions can be prevented, while others are beyond our control.
You may have an increased risk of developing osteoarthritis of the hip if you:
- Are in your late 40s or older
- Are a woman
- Are obese or carrying extra weight
- Have sustained joint injuries at some point in your life
- Regularly subject your joints to stress or trauma
- Have family members with osteoarthritis
- Were born with bone deformities
- Have certain metabolic diseases
- Have conditions such as hip dysplasia that cause structural problems with hip joints
What Are the 4 Stages of Osteoarthritis of the Hip?
There are four stages of osteoarthritis of the hip. Osteoarthritis is generally easier to treat in the early stages of the condition, so it’s important to identify as soon as possible so that prompt treatment can begin.
Treatment options are dictated by which stage of osteoarthritis you’re currently in.
Stage 1: Minor
Stage one is the least severe stage of this degenerative joint disease. At this stage, there will be slight wear-and-tear on the hip joint, but nothing very noticeable. People in stage one of osteoarthritis do not experience pain.
It may not yet be necessary to look at treatment options at this stage; however, a doctor may recommend an exercise routine to manage any symptoms.
Stage 2: Mild
The second stage of hip arthritis may be accompanied by bone spurs. These will be visible as little growths on X-rays.
After long periods of sitting still, the person may experience stiffness or discomfort when they try to move their hip joint.
A new exercise regimen, along with a fitted brace, may form part of your stage two treatment plan.
Stage 3: Moderate
The cartilage that protects the hip joint starts to wear down, decreasing the space between the bone and the joint. This results in the bone rubbing directly against the socket, causing pain during movement.
Treatment options at stage three include over-the-counter and prescription pain medication.
Stage 4: Severe
This is the most severe osteoarthritis stage. It is characterized by the near-complete loss of cartilage around the hip joint and multiple bone spurs, causing pain that makes it difficult to function.
Treatment options for stage four typically involve surgical treatments, such as hip replacement and bone realignment surgery.
Key Point: What Are Some Complications of Hip Osteoarthritis?
If osteoarthritis is not treated or effectively managed, certain complications can arise. Some of these may include:
- Bleeding or infection in the joints
- Pinched nerves
- Loss of stability due to tendon and ligament ruptures
- Osteonecrosis (bone death caused by poor blood supply)
Osteoarthritis may also result in long-term effects that impact your quality of life. These may include:
- Loss of productivity
- Disrupted sleep patterns
- Fatigue
- Anxiety and depression
- Social isolation
- Weight gain
How is Hip Osteoarthritis Diagnosed?
Your doctor will need to rule out other causes of hip pain before they diagnose osteoarthritis. To do this, they will ask you questions about your medical history and then conduct a physical examination.
During the physical examination, the doctor will do a series of tests and search for symptoms of hip arthritis.
There is currently no lab test that can determine the presence of osteoarthritis, but tests can be used to rule out other conditions.
Some diagnostic tools doctors may use to help determine whether someone has osteoarthritis, include:
- X-rays: From an X-ray, doctors can identify bone spurs and determine cartilage loss by looking at the space between the joint’s bones.
- MRI (magnetic resonance imagining) scans: Though more costly and time-consuming than X-rays, MRIs allow doctors an in-depth look at bones and soft tissues, such as cartilage, tendons, and muscle. These scans are used to exclude the presence of other conditions.
- Ultrasound: These can be used to identify cysts that are common in those with osteoarthritis. An ultrasound can also assess tendons and ligaments, which can be damaged due to osteoarthritis.
A variety of lab tests can be done to determine the presence of other conditions that may be causing joint pain, such as rheumatoid arthritis.
What Causes Hip Osteoarthritis?
Some causes of osteoarthritis of the hip can be prevented, while others are out of our control. Being mindful of activities that affect the joints can help decrease your risk of developing severe hip arthritis.
Osteoarthritis can be caused by:
- Genetics: If you are born with joint abnormalities or osteoarthritis runs in the family, you may be more prone to developing hip osteoarthritis.
- Injuries: Hurting your joints or back increases the likelihood of developing osteoarthritis.
- Joint stress or overuse: Whether due to your job, extracurricular activities, or lifestyle factors (such as being overweight), your joints may be taking extra strain that contributes to hip arthritis.
- Other diseases or conditions: Certain conditions increase your chances of getting osteoarthritis of the hip. These include rheumatoid arthritis and diabetes.
What Are the Treatments for Hip Osteoarthritis?
Hip arthritis is more easily treated in its earlier stages, so it’s vital to seek professional medical advice if you experience joint pain or stiffness. Don’t wait for the more severe hip arthritis symptoms to appear before getting help.
Although there’s no definitive cure for osteoarthritis, you can find symptomatic relief with treatment.
Lifestyle modifications
Exercise
You can help relieve the symptoms of osteoarthritis with a good exercise routine. Some activities that are great for osteoarthritis include:
- Swimming
- Walking
- Biking
- Yoga
- Gentle stretching exercises
- Household chores that keep your joints in motion, such as vacuuming
Be sure to start slowly and consult a doctor before implementing any strenuous exercise programs.

Weight reduction
Maintaining a healthy weight can help preserve your joints. When you carry less weight, your knees and hips will take less strain, which reduces the swelling and inflammation associated with osteoarthritis.
Eating a balanced diet
By consuming foods that provide your body with the right nutrients, you can help relieve osteoarthritis symptoms.
Some foods you can incorporate into your diet, and those you should avoid, are listed below:
Foods to Eat
- Oily fish, such as sardines, salmon, and tuna.
- Oils that reduce inflammation. For example, avocado and safflower oil.
- Dairy products rich in protein, calcium, and vitamin D. Good examples include milk, cheese, and yogurt. Those reducing caloric intake should opt for low-fat or fat-free options.
- Dark green vegetables, such as collard greens, spinach, broccoli, and kale.
- Green tea.
- Garlic.
- Nuts.
Foods to Avoid or Limit
- Processed sugars, especially those included in soda, candies, sweetened tea, and flavored coffees.
- Foods high in saturated fats. Examples include red meat, deep-fried foods, and takeout meals.
- Refined carbohydrates such as bread, pasta, cereals, pastries, white rice, and potato chips.
Medications
Your doctor will be able to prescribe medication that can ease the pain and discomfort of osteoarthritis.
Some medications include:
- Hyaluronic acid injections
- Corticosteroids (steroids such as cortisone and prednisone)
- Creams and ointments containing menthol or capsaicin
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen
- Analgesics such as Tramadol
Physical therapy
Working with a physical therapist can help:
- Increase the range of motion in your joints
- Strengthen the muscles that support the affected joint
A physical therapist can also teach you how to safely perform exercises that will help relieve the symptoms of hip osteoarthritis.
Walking aids
A walking aid can take the pressure off tender or swollen joints and decrease your risk of falling.
Examples of walking aids include:
- Canes
- Crutches
- Braces
- Walking frames
- Shoe inserts (orthotics)

Surgical treatments
If lifestyle changes and medication are not enough to relieve the symptoms of hip arthritis, there are surgical treatment options available.
Orthopedic surgeons may recommend one of the following surgeries to help you regain mobility and reduce pain.
- Hip resurfacing: The damaged hip bone and cartilage will be trimmed and capped with a metal shell.
- Total hip replacement surgery: An artificial ball-and-socket joint will be used to replace the affected joint. This is also known as joint replacement surgery; it can be performed on other parts of the body that are damaged by arthritis, too — for example, the knees.
- Bone realignment surgery: Also called an osteotomy, this surgical treatment option involves cutting and reshaping the hip’s ball joint and placing it back into the socket.
Alternative therapies
For those who aren’t ready for invasive surgery or who’d like to try alternatives to OTC and prescription medicine, there are other options.
Alternative treatments for osteoarthritis include:
- Turmeric supplements
- Acupuncture
- Tai chi
- Products containing cannabidiol (CBD)
- Massage therapy
When Should I See a Doctor for Osteoarthritis of the Hip?
Because osteoarthritis is a degenerative disease, it is best to seek help as soon as you notice something going on with your joints — such as hip discomfort, a decreased range of motion, weakness, instability, or pain.
It is especially important to seek treatment if you experience these symptoms after an injury, have a family history of arthritis, or you’re above the age of 40.
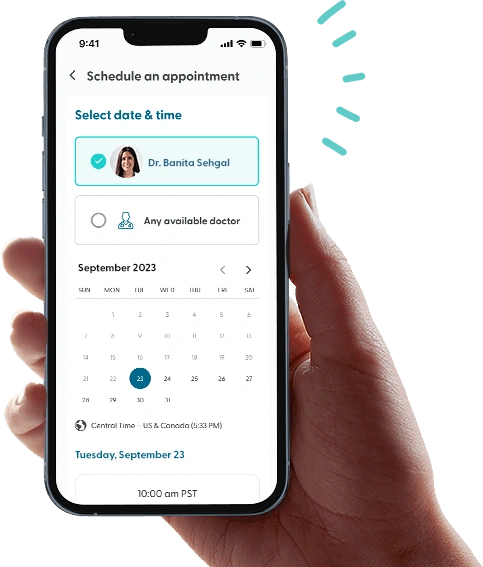
With LifeMD, you can consult with a board-certified doctor or nurse practitioner, right from home. Head over to LifeMD to make a video appointment.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD today and experience amazing healthcare, discounted labs and prescription medications... plus around-the-clock access to medical guidance.