A Comprehensive Overview of Menopause and Weight Gain
Weight changes during the menopausal transition are extremely common and can feel confusing or frustrating, especially when you’re already navigating physical and emotional shifts. Understanding why weight gain happens, and what you can realistically do to support your metabolism, can make this phase of life far more manageable.
This article explains what truly happens to the body during perimenopause, the moment of menopause, and postmenopause, and offers practical strategies to support metabolic health, body composition, and overall well-being.
Understanding Menopause
Many sources define menopause incorrectly. Menopause is one single day marking 12 consecutive months without a menstrual period. After that day, a woman is postmenopausal.
The years leading up to that day are called perimenopause, and this is when most of the hormonal changes occur. Perimenopause can last several years, and it’s during this time that many women begin noticing symptoms, including weight gain.
After menopause, the body shifts into a new hormonal baseline as ovarian hormone production declines significantly.
Understanding this timeline is essential because most metabolic changes originate in perimenopause, not menopause itself.
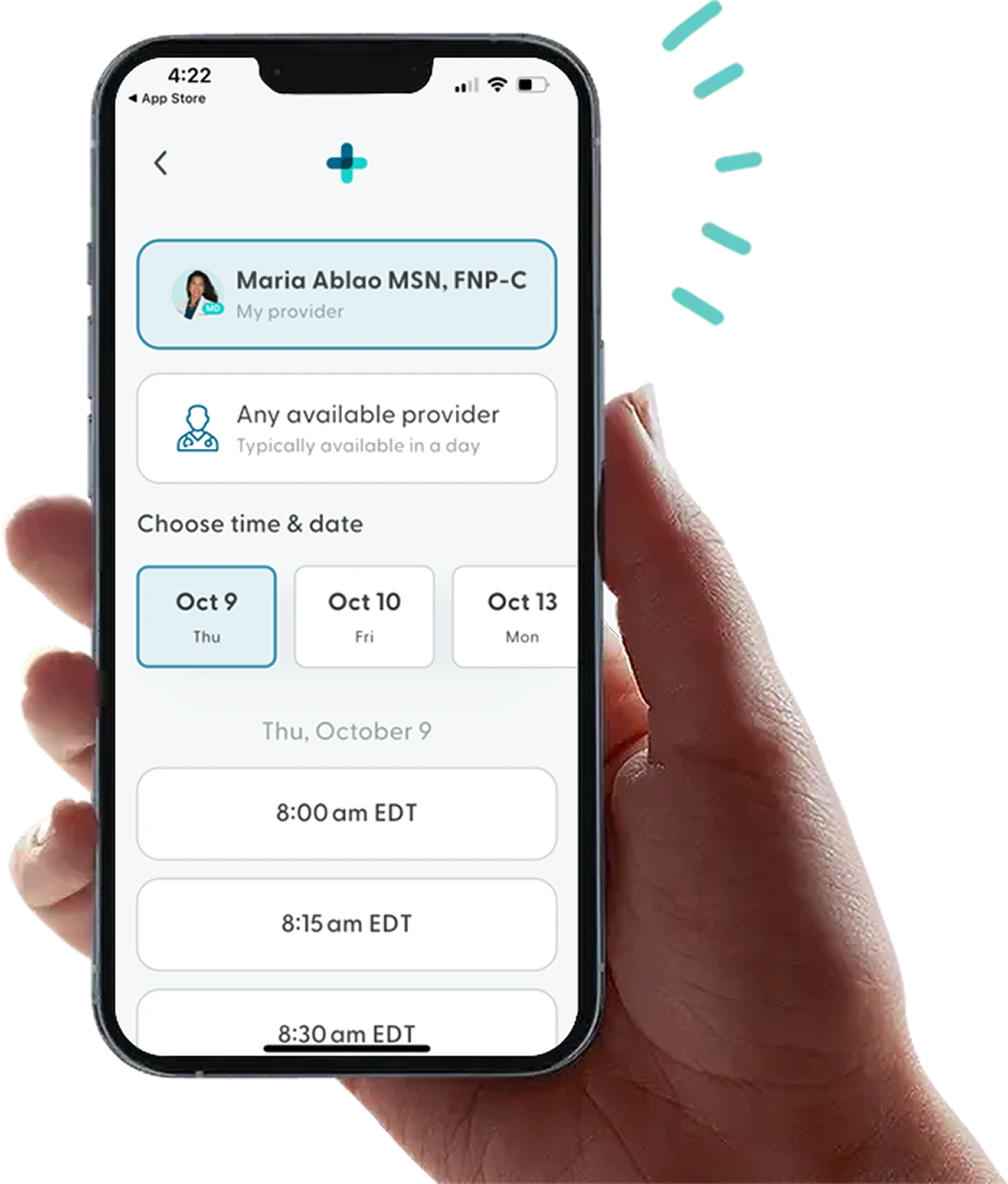
Feel like yourself again
A licensed provider can help you understand your symptoms and determine if hormone replacement therapy is the right next step.


Why Weight Gain Happens During the Menopausal Transition
Weight gain during perimenopause and postmenopause is not simply about “aging.” Instead, it results from several overlapping physiological changes that influence metabolism, muscle mass, appetite, fat distribution, sleep, and stress hormones.
Declining estrogen and body composition changes
Estrogen plays a meaningful role in:
Supporting muscle mass
Influencing where fat is stored
Helping regulate appetite, insulin sensitivity, and metabolic rate
As estrogen decreases, the body tends to shift toward central fat storage (belly region) and may lose lean muscle more quickly. With less muscle, metabolism slows, making it easier to gain weight even without increasing calories.
Changes in progesterone and sleep quality
Progesterone naturally decreases during perimenopause. Because progesterone has calming effects and supports sleep, lower levels may contribute to:
More nighttime awakenings
Lighter, fragmented sleep
Poor-quality sleep alters hunger hormones and increases cravings, particularly for sugar and refined carbohydrates.
Age-related muscle loss, accelerated by hormonal shifts
Muscle mass naturally declines with age, but this decline accelerates during the menopausal transition. Less muscle means fewer calories burned at rest, which can make weight maintenance more challenging.
Increased insulin resistance
Hormonal shifts, combined with changes in body composition, may reduce insulin sensitivity. This can increase cravings, raise blood sugar levels more easily, and contribute to abdominal fat gain.
Heightened stress response
Many women in midlife experience increased stress due to work demands, life transitions, caregiving, and aging parents. Chronically elevated cortisol promotes abdominal fat storage and makes weight loss more difficult.
Changes in lifestyle and daily movement
Joint discomfort, fatigue, or disrupted sleep may reduce physical activity levels during this time of life. Even small reductions in daily movement can accumulate and influence weight over time.
When Does Menopausal Weight Gain Begin?
Most women notice changes during perimenopause, when hormones begin fluctuating. This may start in the early to mid-40s, though some women experience it sooner or later. Because this stage can last several years, metabolic challenges can accumulate gradually.
Once menstruation stops and a woman becomes postmenopausal, the hormonal landscape is more stable, though metabolism continues to evolve.
What are the Risks Associated With Menopausal Weight Gain?
It’s important to understand that while weight gain has its risks, the location and physiological effects of that weight can also heavily influence health. An increase in central (abdominal) fat is associated with a higher risk of:
Cardiovascular disease
Insulin resistance and type 2 diabetes
High blood pressure
Worsening lipid profiles
Joint discomfort and osteoarthritis
Sleep disturbances
Reduced mobility
Increased inflammation
Psychological effects are also common. Weight gain may affect confidence, body image, and emotional well-being, especially during a phase of life that already involves transition.
Managing weight during perimenopause and postmenopause also helps to protect long-term health, maintaining strength, supporting energy, and feeling well in your body.
Strategies That Support Healthy Weight and Metabolism During Menopause
While the menopausal transition changes the metabolic landscape, there are many effective strategies that help support weight regulation, muscle mass, and overall health.
Get prescription weight loss medication online.
Find out if you're eligible for GLP-1s, and get started on your weight loss journey for as low as $75/month.


Prioritize a balanced, nutrient-dense diet
Choosing foods rich in protein, fiber, healthy fats, and minimally processed carbohydrates helps maintain muscle, stabilize blood sugar, and regulate appetite.
A nutrient-dense approach may include:
Lean proteins (fish, poultry, eggs, tofu, legumes)
Non-starchy vegetables
Whole fruits
Healthy fats (avocado, nuts, seeds, olive oil)
Whole grains and starchy vegetables in balanced portions
Protein is especially important, as it supports muscle preservation and helps regulate hunger. Many women need more protein during midlife than they did in their 20s and 30s.
Mindful eating and portion awareness can also help prevent unintentional calorie surpluses, particularly during times of hormonal variability.
Emphasize regular physical activity
Movement is one of the most powerful tools for supporting metabolic health during perimenopause and postmenopause. The combination of strength training, aerobic exercise, and mobility work is especially effective.
Beneficial forms of exercise include:
Strength and resistance training: Helps build and preserve muscle, improve insulin sensitivity, and increase metabolic rate.
Aerobic exercise: Activities like walking, jogging, swimming, or cycling support cardiovascular health and calorie burn.
Mobility and flexibility work: Yoga, stretching, or Pilates can reduce stiffness, support joint function, and enhance recovery.
A balanced exercise routine not only helps manage weight but also improves mood, sleep quality, and energy levels.
Support stress regulation
Chronic stress increases appetite and cravings, raises cortisol levels, and promotes fat storage around the abdomen. Incorporating stress-management practices can have a direct effect on metabolic balance.
Helpful strategies include:
Mindfulness or meditation
Deep breathing techniques
Yoga, tai chi, or gentle movement
Time in nature
Creative hobbies
Social connection
Even a few minutes of daily stress support can improve resilience and hormonal balance.
Prioritize high-quality sleep
Poor sleep amplifies nearly every challenge of the menopausal transition – including cravings, appetite, mood changes, and weight gain.
To improve sleep quality:
Maintain a consistent sleep–wake schedule
Limit screens and bright lights before bed
Keep the bedroom cool and dark
Avoid heavy meals late at night
Reduce caffeine and alcohol intake
Establish a relaxing bedtime routine
Supporting sleep allows the body to regulate appetite hormones more effectively and enhances metabolic stability.
Build support and accountability
Menopausal transitions are easier to navigate with support. Sharing your journey with others can reduce feelings of isolation and help maintain motivation.
Support may come from:
Friends or family
Community groups
Online forums
Healthcare providers
Nutrition or lifestyle professionals
Regular check-ins, whether formal or informal, can provide encouragement and keep goals on track.
Can Hormone Therapy Help With Weight Management?
Hormone replacement therapy (HRT) can be very helpful for alleviating symptoms like hot flashes, sleep disturbances, mood changes, and vaginal dryness. Because hormone therapy restores some estrogen, it may also have indirect benefits on metabolic health, muscle preservation, and fat distribution.
Whether hormone therapy is appropriate depends on individual health history, symptom severity, and personal goals. A healthcare provider can help determine the safest and most effective approach.
Can Menopausal Weight Gain Be Prevented?
Weight gain during the menopausal transition is common, but not inevitable. Some women maintain their weight with consistent lifestyle habits, while others have more difficulty due to genetics, stress levels, sleep quality, and overall hormonal shifts.
Starting supportive habits early in perimenopause, or even before, can make weight changes more manageable.
Even if weight gain cannot be fully prevented, many women successfully minimize it and protect their long-term health through daily movement, high-quality nutrition, stress support, and adequate sleep.
Maintaining Realistic Expectations and a Positive Mindset
This stage of life involves change, and weight is often part of that change. Setting realistic goals and practicing self-compassion are essential for emotional well-being and long-term success.
A supportive mindset may include:
Acknowledging that the body naturally evolves with age
Focusing on health rather than perfection
Celebrating non-scale victories such as energy, sleep, mood, and strength
Approaching weight management as a sustainable lifestyle, not a quick fix
Cultivating appreciation for your body, even as it changes, can make this transition more empowering and far less stressful.
Learn More about Menopause and Weight Management
If you’re concerned about weight management or want to know more about how it can affect women throughout the menopause transition, LifeMD is here to help.
Hormone replacement therapy (HRT) may be an effective option for some women, helping to reduce hot flashes, improve sleep, and support bone health. The LifeMD Women’s Health Program offers personalized HRT plans, virtual consultations with licensed providers, and convenient access to lab testing and prescriptions tailored to your unique needs.
LifeMD also offers a Weight Management Program for qualifying patients. The program includes access to GLP-1 medications like the Wegovy pill combined with ongoing support from a team of licensed clinicians.
Make an appointment with LifeMD to help kickstart your journey towards a healthier you.
More articles like this
Feel better with LifeMD.
Your doctor is online and ready to see you.
Join LifeMD for seamless, personalized care — combining expert medical guidance, convenient prescriptions, and 24/7 virtual access to urgent and primary care.
GLP-1
Zepbound® Wegovy® Saxenda®
This is it! Be part of the weight loss movement everyone’s talking about.
Get Started Now
 Medically reviewed and edited by
Medically reviewed and edited by 








